Combating COVID-19 has required unprecedented global efforts and innovation across multiple systems, including healthcare. As restriction ease in the U.S., those in the industry are considering which changes are worth carrying forward. This article examines pandemic-prompted advancements in behavioral and mental health worth keeping as restrictions ease and potential improvements for future care.
Four Key Advancements
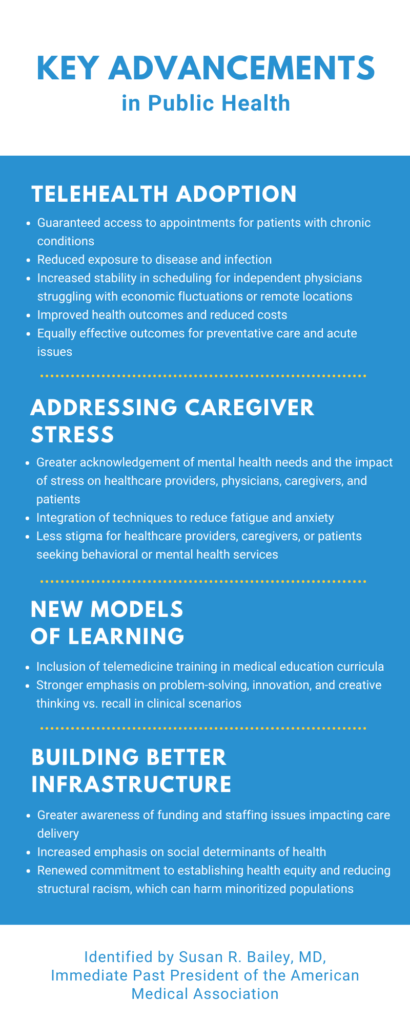
Susan R. Bailey, MD, Immediate Past President of the American Medical Association, recently identified four key advancements in public health necessitated by the pandemic in the following areas:
- Telehealth adoption
- Addressing caregiver stress
- New models of learning
- Building better infrastructure
All four of these areas, which directly impact behavioral and mental health delivery, should be preserved post-pandemic and expanded upon, according to Dr. Bailey, because they have been proven to benefit patients and healthcare providers in the following ways:
Preserving these advancements and even building upon them requires commitment and coordination at the local, state, and federal levels. Although it will likely be challenging, ensuring these advancements are not abandoned as we return to “normal” can help provide better services going forward.
Post-Pandemic Realities
One of the inescapable realities of COVID has been the impact it has had on people’s mental health. Depression, anxiety, and substance use all rose significantly in 2020, with professionals seeing a significant jump in psychiatric symptoms – even among people with no history of mental illness.
Among adolescents, providers have seen a dangerous rise in mental health-related ER visits. This was confirmed by data from the Centers for Disease Control (CDC), which also noted an increase in persistent sadness or hopelessness among U.S. high school students during their survey.
Another group whose mental health was severely influenced by the pandemic were parents with children under 18 and unpaid caregivers of adults. According to the CDC, these individuals have been and continue to struggle with increases in depression, anxiety, and suicidal thoughts.
Further Transformation
The mounting evidence at the state and national level all points to the same conclusion: our post-covid focus priority will be behavioral and mental health services.
In addition to keeping all of the advances noted above, another emerging strategy gaining support is integrated care. Integrated care combines physical care with behavioral and mental health interventions—all of which are available within the same facility.
This strategy, also sometimes referred to as a Collaborative Care Model (CCM), has proven effective in randomized trials for improving patients’ outcomes for physical, mental, and behavioral health. In addition, cost analyses have shown that this practice not only controls costs, but typically yields a return of $12.75 for every $1 invested.
As more people become aware of the looming behavioral and mental health needs of the U.S. population post-pandemic, public health advocates and legislators have begun considering structural changes to our healthcare system designed to optimize integrated care. These include:
- Requiring school-based mental health awareness education programs to reduce stigma and integrating mental health services in schools to increase access;
- Establishing a single licensing regulatory framework so that mental, behavioral, and physical health care providers are no longer regulated as separate entities;
- Approving a permanent extension of telehealth/telemedicine payment allowances at the federal level and investments in national broadband access;
- Allowing mental health services to be provided at urgent care centers and encouraging coordination between emergency rooms and psychiatric follow-up providers; and
- Overhauling payment systems and funding methods to improve care delivery.
The increased need for behavioral and mental health services across multiple demographics in the U.S. will require collaboration and innovation. Integrated care may be one of the unanticipated outcomes of the COVID-19 pandemic that shapes our nation’s “new normal.”

