Officials have begun to discuss ending the public health emergency declaration previously required by the COVID-19 pandemic. The end of emergency status would put an end to several federal funding strategies and special programs put in place to help protect disability programs throughout the United States. In this article, we explore the potential consequences the expiration could have for Medicaid and people with intellectual and developmental disabilities (I/DD).
Temporary Changes Due To Public Health Emergency
One of the primary changes afforded by the declaration of a public health emergency has been the ability for states to access additional federal funding for existing Medicaid beneficiaries. In addition, providers of home- and community-based services (HCBS) were given increased flexibility with regard to staffing in order to maintain a consistent level of care during the pandemic.
Currently, the public health emergency status has been extended through July 15, 2022, by the U.S. Secretary of Health and Human Services, Xavier Becerra. The White House has provided no indication as to whether the emergency status will be extended beyond that date. However, a fact sheet published by the Administration for Community Living (ACL) under the Department of Health and Human Services (HHS) is recommending people with I/DD and other disabilities begin to prepare for an expiration.
Medicaid Changes Upon Expiration
The ACL fact sheet, titled “Preparing for Medicaid Changes When the Public Health Emergency Expires” provides guidance for both providers and Medicaid beneficiaries, beginning with the following advice:
“When the federal declaration of a public health emergency (PHE) expires, many of the flexibilities initiated during the PHE will need to be rolled back. This return to pre-pandemic operations will have far-reaching impacts for older adults and people with disabilities. Changes in Medicaid enrollment and eligibility will be particularly important—and potentially confusing or disruptive—for current enrollees.”
One of the key changes that will result from the expiration of emergency status is the end of a “continuous coverage” provision required by the Families First Coronavirus Response Act (FFRCA), which was enacted in March of 2020. FFCRA guaranteed additional federal dollars for Medicaid programs if they committed to keeping beneficiaries enrolled, even if they might normally become disenrolled due to a change in “categorical eligibility” or a rise in income.
Recommended Steps
Although a firm expiration date is not clear, the White House has said that states can expect to receive notice of the expiration at least 60 days in advance. Once the public health emergency is declared over, the continuous coverage provision will end. States will then have one year to evaluate beneficiaries for eligibility.
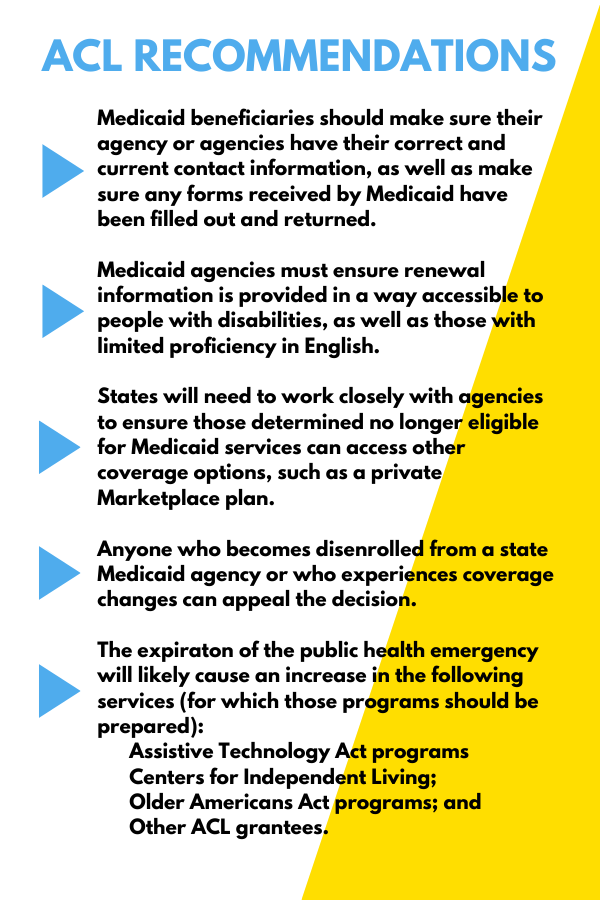
To facilitate this process, the ACL has recommended the following steps: