A new assessment tool measuring social determinants of health (SDOH) for people with intellectual and developmental disabilities (I/DD) has been developed and piloted by a Los Angeles County Meds-Peds speciality clinic “within a large, diverse academic health system.” Results of the pilot were recently published via Cereus’s Meds-Peds Academic Channel. In this article, we summarize the pilot’s purpose, design, key findings and considerations for other providers interested in using the SDOH screening tool.
Pilot Background & Purpose
The COVID-19 pandemic proved particularly dangerous for individuals with I/DD. This included the one in six U.S. children with I/DD, who “experience disproportionate rates of immune, metabolic, cardiovascular, and neurological disorders, as well as anxiety, depression, functional somatic symptoms, and other co-occurring physical and mental health conditions” – all of which were exacerbated by the pandemic.
One known influence on the health outcomes for individuals with I/DD has long been SDOH. These are described as “the underlying social, economic, and environmental conditions that lead to poor health outcomes and high healthcare costs.” In order to better serve the needs of children with I/DD and their families, the researchers of this study developed a five-item screening tool for SDOH that could be used within their Meds-Peds clinic and an affiliated primary care practice.
The new SDOH screener included “five items from the Accountable Health Communities (AHC) Health-Related Social Needs Screening Tool (HRSN).” Specifically, the tool was used to gauge the following for children in the pilot study:
- Experience(s) of social isolation;
- Determination of food security or insecurity;
- Transportation needs; and
- The ability to pay housing and medical care, among other basic needs.
Although research has shown that “SDOH screening and referral in primary care have been found to increase receipt of social services among patients with I/DD,” it has also shown that “screening activities may decline after initial training and education surrounding utilizing the screener.” Thus, the authors of the study hoped to not only pilot new workflows that might make screening more scalable, but also “to highlight the challenges and opportunities identified during the mid-way point of implementation and pilot testing.”
Study Design
Data was collected between October 2022 and April 2023 from 747 patients who received care through either the Los Angeles County Leadership Education in Neurodevelopmental Disabilities (LEND) clinic or the primary care practice. The LEND clinic is one location among 60 currently located in the U.S. and conducts all patient visits via telehealth. Both the clinic and the private practice serve “a significant Hispanic population (49.1%) as well as a significant proportion of individuals living in poverty (14.1%).”
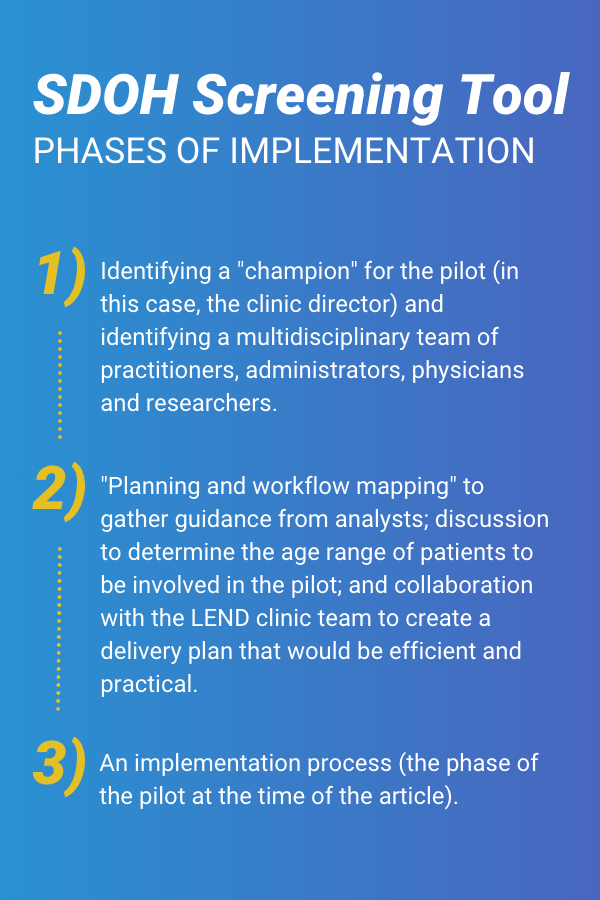
To facilitate use of the screening tool, the developers worked with IT experts on creating “an automated process for electronic release” with all patients prior to their visit. To ensure for quality improvement, the team also followed three phases for implementation:
Tip sheets and both email and in-person reminders were provided to patients to increase the likelihood of completion of the SDOH screening tool.
Key Findings
At the LEND clinic, 94 SDOH screening tools were provided to patients; however, only 9 were completed, “yielding a 10% response rate.” The mean age for completed screener was 15.4 years. Of the total completed, 5 were identified as “positive,” which resulted in “referrals to community-based organizations.”
At the primary care clinic, 2,522 SDOH screening tools were provided to patients, and 738 were completed. This yielded a response rate of 43%, and the median age of respondents was 37.72. Of the completed screeners, 143 were identified as positive, resulting in “referrals to community-based organizations.”
Based on the low response rate at the LEND clinic, the study authors noted the following changes to implementation that might “maximize the uptake among the I/DD population”:
- Improving accessibility for the SDOH screener through the inclusion of a “walk-through video” within the reminder email that is sent to patients before their appointments. The video provides detailed instructions “utilizing multiple modalities (e.g., visual and oral cues via clear narration, captioning, and graphics).”
- Adding a virtual waiting room that can be customized for patients with an additional reminder if they have not yet completed the SDOH screener. This virtual space will be provided to patients the day of their appointment and will include “virtual signage and instructions for accessing and completing the screener.”
- “Soliciting feedback from all LEND clinicians about the services, supports, and resources they refer patients to following positive SDOH screens.”
Additional Considerations
In addition, the study authors provided three recommendations for “national efforts to implement, test, and scale universal SDOH screening and referral practices in Med-Peds”:
- Establish and utilize a multidisciplinary team throughout.
- Maintain a quality improvement process “that is continuously and iteratively revised.”
- “Forge multi-site collaborations and learning networks focused on SDOH screening and referral.”
For the next phase of their research, the study authors will be focusing on “effective wide-scale SDOH screener adoption within our larger health system and potentially across the 60 LEND clinics nationwide,” as well as encouraging clinics outside their system to utilize the screener. Researcher-provider partnerships may be the key to building a sustainable and scalable approach so that data can be collected, interpreted, and shared across the country for the benefit of patients with I/DD.
“We call on additional Med-Peds healthcare teams without universal SDOH screening protocols in place, particularly those serving the I/DD population, to consider adopting these practices and build a learning network to bolster their effectiveness.”
To read the full, peer-reviewed article about the pilot, click here.

